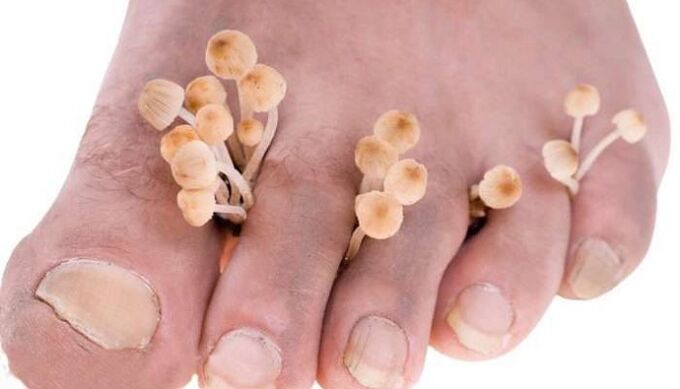
The skin between the toes is often prone to fungal infections. This problem is common among people who lead an active lifestyle and is quite burdensome and unpleasant. Considering the high relevance of foot mycosis, more attention should be paid to them.
Causes of itching and scaling in the interdigital folds
Toes itch and peel due to various disease processes - allergic reactions, scabies, eczema - but for many people these symptoms arise from a fungal infection. The epithelium becomes wet and cracked with mycosis of the feet, which is a separate nosology in dermatology. It is caused by pathogenic fungi that affect smooth skin and nails. The infection is caused by several pathogens:
- Trichophyton (T. rubrum, T. interdigitale, T. violaceum).
- Epidermophyton (E. floccosum).
- Mold fungi.
Mycosis is a contagious disease that is transmitted from person to person in places with high humidity (bathrooms, saunas, swimming pools, beaches) through shoes, carpets, benches, etc. infected. Fungal spores are found in large quantities in the horny scales of the epidermis, with which they are transferred.
Predisposing factors
Numerous local and general factors contribute to skin lesions, increasing the likelihood of developing a fungal infection between the toes. The former include the following:
- Excessive sweating (hyperhidrosis).
- Incorrectly selected shoes (uncomfortable, made of synthetic materials).
- Anatomical characteristics of the foot (flat foot, narrow creases).
- Presence of abrasions and diaper rash.
- Injuries (mechanical, chemical).
The role of systemic disorders is explained by a decrease in the resistance of the skin barrier and a weakening of the immune defense. Metabolic neurotrophic, vascular and endocrine diseases (polyneuropathy, angiopathy, atherosclerosis, diabetes mellitus, hypovitaminosis) have a negative impact. In addition, the role of weather conditions (high temperature and humidity) and the virulence of the pathogen is noted.
Mycosis of the foot with skin lesions between the toes is caused by a fungus and develops against the background of local or systemic disorders.
What does mycosis look like?

Mycosis begins in the skin of the interdigital folds, but then spreads to other parts of the foot: the sole, back and lateral surfaces. In clinical practice there are different forms of fungal infection:
- Scaly.
- Intertriginous.
- Dyshidrotic.
The scaly form begins with mild redness and light flaking. They may be limited to only certain areas or become widespread. This form often goes unnoticed by the patient himself and therefore is the most dangerous from an epidemiological point of view. The fungus initially affects one foot, but can later spread to the healthy part.
As it progresses, the scaly form can transform into a dyshidrotic form, characterized by an acute course with allergy of the body and the formation of blisters on the arch of the foot. Combining, they form multichambered blisters, which, after opening, leave eroded foci surrounded by a border of exfoliated epidermis. Spreading to the lateral surfaces of the foot, the process combines with the intertriginous form. As epithelialization occurs, the areas dry out, becoming scaly again.
Outbreaks of fungal infection are often accompanied by itching. It arises from the interdigital folds in the most common form - intertriginous, occurring independently or against the background of the squamous. Usually the process begins between the IV and V fingers (less often III and IV). Cracks appear there, surrounded by a border of exfoliated epidermis. The fungus can spread to other creases, toes, and the back of the foot. Subsequently, crying with painful erosions occurs.
The disease is characterized by a long course with periodic exacerbations that occur in the warm season. Bacterial flora penetrates more easily through the loosened stratum corneum of the epidermis, so the intertriginous form can be complicated by streptococcal infection with the development of erysipelas and thrombophlebitis.
Damage to the interdigital spaces often occurs in combination with other forms of mycosis of the foot, which indicates the unity of pathological processes.
Diagnostics
The disease has a rather characteristic clinical picture, so the initial diagnosis is made based on the results of a medical examination. To identify the pathogen, microscopy and culture of scrapings from the affected skin are used. The presence of a systemic pathology contributing to the development of mycosis is confirmed by additional methods: a biochemical blood test (glucose, hormonal spectrum, immunogram), ultrasound examination of the lower extremities, etc.
How to treat the sore?

To effectively eliminate the fungus, it is first necessary to eliminate the conditions that create favorable conditions for its development. If your foot itches and feels sore, it is advisable to pay attention to the following advice:
- Wear comfortable, breathable shoes.
- Wear cotton socks.
- After showering and bathing, dry your feet.
- Use personal slippers in public places.
In the treatment of mycosis of the foot, attention is paid to abandoning bad habits, a healthy diet (reduction of animal fats, sweets, including fresh vegetables, fruits, lactic acid products in the diet), hardening.
In addition to general recommendations that have a therapeutic and prophylactic focus, traditional medicine actively uses pharmacological means of correction, without which it is not possible to cure mycosis. Therapy can be external or systemic.
Effective creams and ointments
It is necessary to fight the infection with specific drugs that act against toe fungus. For the scaly form, the doctor prescribes various creams and ointments, including various antifungals. If there are dense foci of hyperkeratosis on the soles of the feet, treatment begins with exfoliating procedures with salicylic acid, lactic acid, resorcinol and collodion. At night, a medicine intended for external use is placed under the bandage. It contains salicylic acid, which has anti-inflammatory, keratolytic and antiseptic properties, and in the morning you take a bath with soap and soda, after which the horny masses will be better removed.
If your skin gets wet and chapped

External treatment of the dyshidrotic form with exudation and cracking begins with lotions with boric acid and potassium permanganate. The interdigital spaces are treated with aniline dye solutions, a product for external use intended for the treatment of various skin diseases. The solution contains components that promote rapid wound healing, eliminate inflammatory manifestations and fight pathogenic microorganisms. After the acute inflammatory process is eliminated, antifungal ointments and pastes are applied to the affected areas. For secondary pyoderma, drugs with antibacterial components are prescribed.
In case of fungal lesions of the skin of the feet, external therapy with antifungal agents, antiseptics and antibiotics is of decisive importance.
Pills
If local agents are ineffective, it is necessary to switch to drugs for internal use. Prescribed antifungal drugs include an antifungal drug, an antifungal drug that has a broad spectrum of action against fungi that cause skin, hair and nail diseases, a drug for the treatment of fungal infections, an antifungal drug. When allergy the body, antihistamines (an antihistamine drug intended for the treatment of allergic reactions) and desensitizing agents (calcium gluconate, sodium thiosulfate, magnesium sulfate) are used. Streptococcal infections can be treated with antibiotics that do not have an activating effect on the microbial flora.
What can be done with folk remedies?
Some traditional medicine methods can be an addition to standard therapy. To treat foot fungus, baths with simple and inexpensive remedies are often used:
- Apple cider vinegar (1 glass per 3 liters of warm water) and soda (5 tablespoons).
- Potassium permanganate (1 g per 2 l).
- Calendula flower decoction (250 g per 2 l).
It is recommended to immerse your feet in the prepared solution for 20 minutes. Additionally, you can apply a drop of tea tree essential oil to the skin between your toes and then wear cotton socks.
Fungus between the toes is a problem that affects many people. To get rid of it as quickly as possible, do not look for possible solutions yourself, it is better to consult a doctor, undergo a diagnosis and receive treatment with a guaranteed result.
















